At the time of posting, several news outlets have posted that more than 80% of patients that were hospitalized due to COVID-19 were found to be Vitamin D deficient.
November 19th, 2020

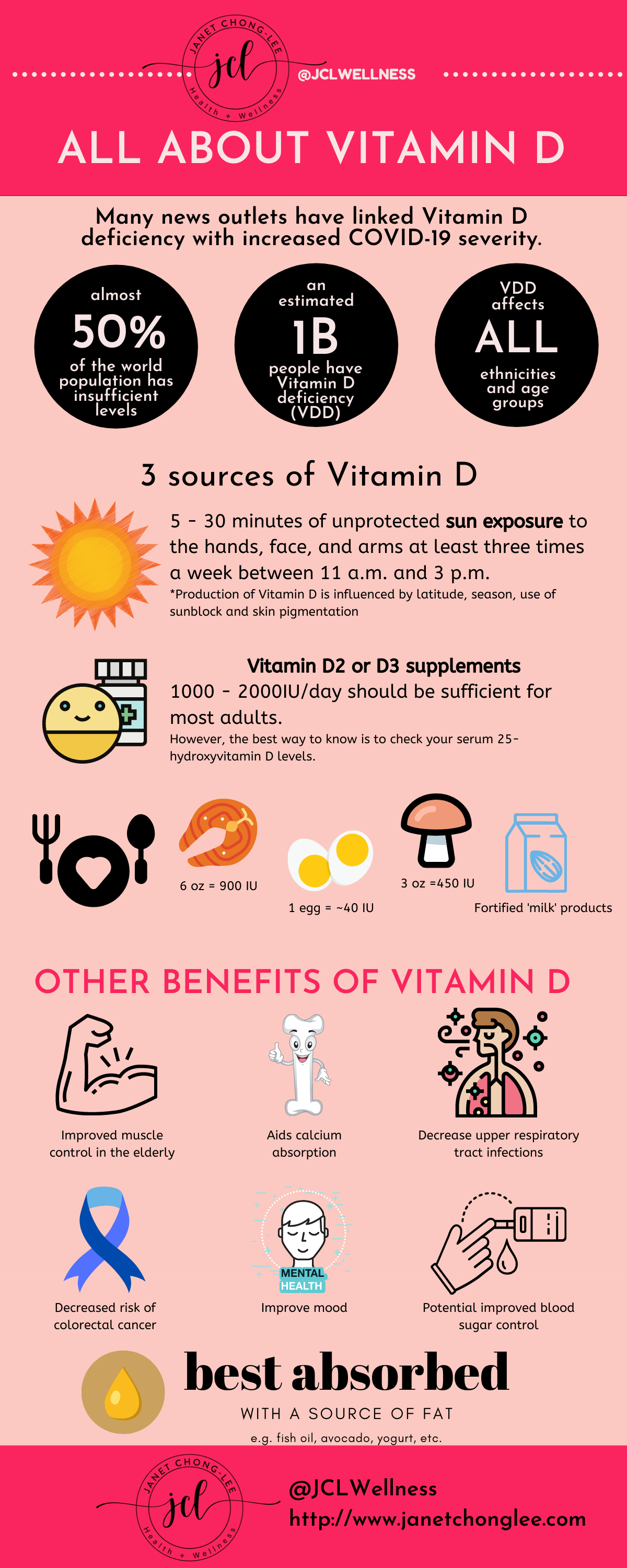
At the time of posting, many news outlets have linked Vitamin D deficiency with increased COVID-19 severity. In one study, more than 80% of patients who were hospitalized for severe COVID-19 had Vitamin D deficiency. Could taking Vitamin D somehow prevent or reduce the severity of COVID-19 infections?
TL;DR - While Vitamin D is not a panacea for every ill or disease, most individuals do not get enough Vitamin D and should consider supplementation if there is limited sunlight exposure. Vitamin D goes beyond bone health, and is involved in immunity, brain health, and insulin sensitivity, among others. While there are currently no double-blinded randomized control trials (the gold standard for evidence based medicine), the studies that are currently available do suggest a link between Vitamin D deficiency and severity of COVID-19 infections. While Vitamin D requirements are unique, 2000IU daily should be sufficient enough to meet the needs of 95% of individuals.
Please read on to learn more about fantastic Vitamin D!
Vitamin D is a fat-soluble nutrient. It is one of the 24 micronutrients critical for human survival. The sun is the major natural source of the nutrient, but vitamin D is also found naturally in fish, eggs, and mushrooms. It is also added to dairy products.
Most of us are familiar with the role of Vitamin D in bone health (it helps to regulate calcium and phosphate balance, affecting bone growth and turnover). A lesser known fact is that Vitamin D receptors are also expressed on immune cells (not to mention almost every other cell in the body) and is able to influence the immune system response. There is supporting evidence that vitamin D has a proven positive effect on the following, including:
The above benefits usually come from higher levels of vitamin D in the body, which can be usually obtained with roughly 2000 IU/day for most individuals.
Vitamin D (aka Vitamin D3) is actually a hormone. There are 3 main sources of vitamin D: sunlight, certain foods, or supplements. It is known as the "sunshine" vitamin because its synthesis requires a partner in the form of UVB rays. It's made in the body by exposing cholesterol (7-dehydrocholesterol to be exact) + adequate sunlight. Production of Vitamin D is influenced by latitude, season, use of sunblock and skin pigmentation. A series of reactions then occur in the body to form Vitamin D3. It is important to note that there is only a sufficient amount of UV light coming from the sun when the UV index is 3 or higher, which only occurs year-round near the equator.
Vitamin D is stored in the fat cells (as it is a 'fat-soluble' vitamin) and becomes the active form through hydroxylation by the liver (to become 25-hydroxy vitamin D) and kidney (active form: 1,25-hydroxy vitamin D or calcitriol). Thus, if you have kidney issues, you may need to take the activated form of Vitamin D.
Vitamin D2 can be found in plants, while Vitamin D3 are from animal sources.
Plant sources of Vitamin D include:
Animal sources of Vitamin D include:
In Canada, Vitamin D is available in both Vitamin D2 or D3 formulations, with D3 being more popular. The maximum dose available over-the-counter is 1000IU (25mcg). Vitamin D is available separately on its own, but is often sold as a Vitamin D + calcium combination since its role in calcium absorption is most well known. Vitamin D3 is available in 400IU, 800IU, or 1000IU; dosage forms include drops or tablets.
In the United States, Vitamin D3 is available in 400, 800, 1000, 2000, 5000, 10,000, and 50,000 unit capsules.
Generally speaking, 5 to 30 minutes of unprotected sun exposure to the hands, face, and arms at least three times a week between 11 a.m. and 3 p.m. is considered enough to keep blood vitamin D levels out of the deficient range (less than 30 nmol/L or less than 12 ng/mL).
When determining how much sunlight you might need, there are two basic factors to consider.
When the UV index forecast in your area is 3 or higher, people with Fitzpatrick skin types 1 or 2 should keep unprotected sun exposure to less than 10 minutes; skin types 3 or 4, less than 15 minutes; and skin types 5 or 6, less than 30 minutes.
Longer periods of unprotected sun exposure don’t necessarily lead to higher vitamin D production, as the UVB rays will eventually cause the vitamin D in your skin to degrade to an inactive state. This is a safety mechanism that helps protect your body against vitamin D toxicity.
The generally accepted terms that refer to different 'states' of Vitamin D status are:
Vitamin D insufficiency affects almost 50% of the population worldwide, and an estimated 1 billion people have Vitamin D deficiency. Ideally, we want to have 'adequate' or 'high' levels of vitamin D.
There are several reasons why Vitamin D deficiency and insufficiency are so prevalent today:
In one study, there were 2 suggestions for how Vitamin D works in the context of COVID-19.
First, vitamin D supports production of antimicrobial peptides in the respiratory epithelium, thus making infection with the virus and development of COVID-19 symptoms less likely.
Second, vitamin D might help to reduce the inflammatory response to infection with COVID-19. Deregulation of this response, especially of the renin–angiotensin system, is characteristic of COVID-19 and degree of overactivation is associated with poorer prognosis. Vitamin D is known to interact with a protein in this pathway—angiotensin-converting enzyme 2 (ACE2)—which is also exploited by COVID-19 as an entry receptor. While COVID-19 downregulates expression of ACE2, Vitamin D promotes expression of this gene.
In one clinical trial, giving 25-hydroxyvitamin D decreased admission to the ICU in those hospitalized with COVID-19, suggesting that Vitamin D may be able to reduce the severity of this disease.
Approximately 1000IU daily is needed for half of the population to reach 75nmol/L (adequate range), and 1700IU daily is needed for 95% of the population to reach 75nmol/L (adequate range). However, the best way to know is to check your serum (blood) 25-hydroxyvitamin D levels.
Vitamin D is best absorbed with a low-fat (11 g of fat) meal as opposed to a high-fat (35 g of fat) meal or empty stomach. Peak vitamin D levels were found to be 32% higher in subjects consuming a meal with fat compared to a fat-free meal of otherwise similar protein content.
Vitamin D is best absorbed with a low-fat (11 g of fat) meal as opposed to a high-fat (35 g of fat) meal or empty stomach. Peak vitamin D levels were found to be 32% higher in subjects consuming a meal with fat compared to a fat-free meal of otherwise similar protein content.
If you're interested in knowing more about the food you eat, the nutrients it contains, and what you might be missing, I'd love for us to connect and chat! We can work together to increase nutrient density in the food choices we make, identify nutrient deficiencies, and how to address them.
We went over a lot of information for our mighty sunshine vitamin, so I've summarized the important points in this handy graphic:
- Janet
Additional links of interest:
Copyright © 2021 JCL Wellness.
All rights
reserved.